|
Getting your Trinity Audio player ready...
|
The pain starts as a whisper on the outside of your knee, then builds with each step until you can’t run anymore. For thousands of runners in Singapore, this is their first encounter with IT band syndrome. The question that follows is always the same: Can I run with IT band syndrome, or do I need to stop completely?
The answer lies somewhere in between. Understanding that the middle ground makes all the difference between a quick recovery and months of frustration.
What Is IT Band Syndrome?
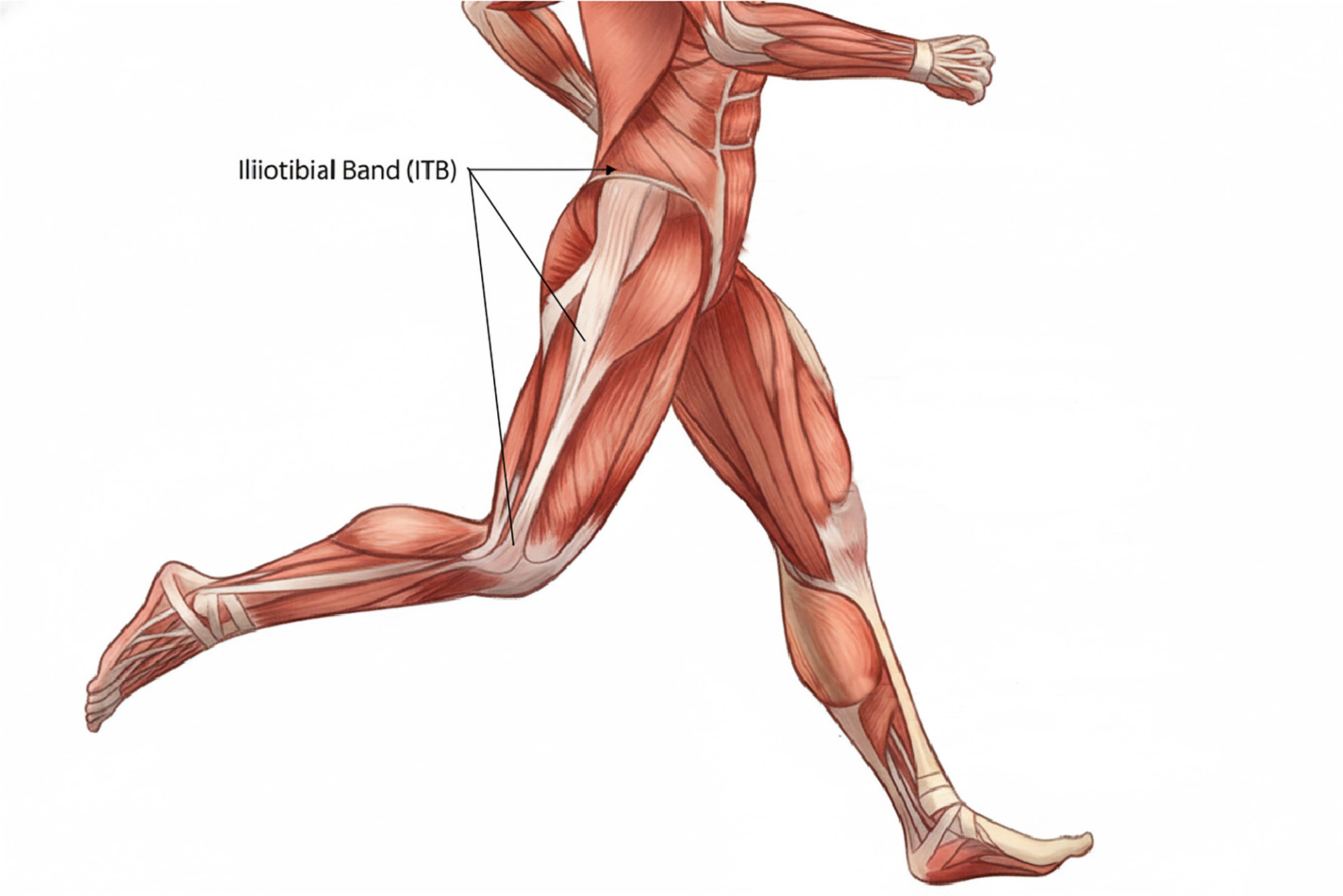
The iliotibial band (or the IT band) is a thick fascial strip that runs from your hip to just below your knee. IT band syndrome occurs when the IT band becomes irritated and inflamed as it crosses the lateral femoral epicondyle.
The anatomical path of the IT band starts at the pelvic bone and runs down the outside of the thigh, crossing the lateral epicondyle of the femur at the knee joint. It acts as a stabilizer for both the hip and knee during movement. This is sometimes referred to as IT band friction syndrome, as it results from repetitive friction or compression of the band as it crosses the lateral epicondyle during flexion and extension of the running stride.
The pain usually shows up on longer runs or when you increase mileage too quickly. This isn’t a simple case of tissue damage that heals with rest alone. The IT band itself doesn’t stretch in any meaningful way, despite what many runners believe.
Symptoms and Diagnosis
Symptoms of IT band syndrome include pain on the outside of the knee that flares up after running or going down stairs. Downhill running is especially problematic as the knee stays slightly bent throughout the stride, keeping the IT band in the exact position where maximum friction occurs.
Some runners describe the pain as a stabbing pain, while others feel a burning or tightness that won’t go away even after they stop moving.
What makes this condition so frustrating is that it feels better after rest, only to come back as soon as you start training again. This pattern convinces many runners they need more time off, and they end up taking extended breaks that weaken the supporting muscles and make the underlying biomechanical issues worse.
Iliotibial band syndrome is one of the most common running injuries. It’s especially common among competitive female runners due to differences in hip structure; a thorough physical examination is necessary. Your physiotherapist will assess your hip and knee alignment, muscle strength and running mechanics to identify the underlying causes of your ITBS.
Why Does IT Band Syndrome Happen to Runners?
Running with IT band syndrome means there’s a breakdown somewhere in the kinetic chain. It’s not just a knee problem. Weakness or dysfunction in the hip muscles directly affects the amount of stress the band experiences with each stride.
Weak hip abductors, especially the gluteus medius, allow the pelvis to drop on the opposite side during single-leg stance. This hip abductor weakness contributes to a contralateral pelvic drop and dynamic knee valgus, which are common problems in runners with IT band syndrome. This Trendelenburg pattern increases hip adduction, which, in turn, increases the angle between the femur and tibia and stretches the IT band more tightly across the lateral knee with every step.
Additionally, weak hip external rotators rotate your femur inward excessively, increasing friction where the band meets the bone. Strengthening these muscle groups, especially the hip abductors and external rotators, is key to preventing IT band syndrome.
Training errors compound these biomechanical vulnerabilities. Increasing weekly mileage by more than 10%, suddenly adding hill repeats, or racing without proper preparation all stress the IT band beyond its capacity to adapt. IT band syndrome accounts for about 8-10% of all running injuries. Even experienced runners preparing for events like the Standard Chartered Singapore Marathon can develop symptoms when they push through fatigue instead of respecting recovery periods.
Running surface matters too. Constantly training on cambered roads forces one leg to work harder to stabilize against the slope and creates asymmetrical loading patterns that predispose that side to injury. Track workouts that always turn in the same direction produce similar imbalances, as they force the runner to utilize one leg more than the other consistently.

Can You Run With the IT Band Syndrome?
You can run with the IT band syndrome, but only if you modify your approach intelligently and address the root causes simultaneously. Rest rarely solves the problem because it doesn’t address the movement patterns and weaknesses that caused the condition. Running through sharp pain or limping through workouts will only deepen the inflammatory cycle and prolong recovery.
You need to consider how much rest your body needs. The key is to find your current pain-free threshold and build from there while implementing a comprehensive treatment plan. Often, a few weeks of reduced activity is necessary to calm down initial inflammation and regain strength before gradually returning to running. Tracking your running distance is a good way to monitor your progress and avoid exceeding your limits. This might mean cutting your run distance in half, avoiding hills entirely, or switching to flat and soft surfaces.
Some runners find that slowing down reduces symptoms enough to maintain fitness while their tissues calm. Others benefit from breaking a single long run into two shorter sessions with several hours in between. Modifying your running style, such as adjusting your cadence or foot strike, can also help manage symptoms and prevent recurrence. Long-distance runners are more prone to IT band syndrome due to the repetitive stress and high mileage involved. When considering stride and biomechanics, pay attention to the leg moving behind the body and then swinging forward for propulsion, as this can affect IT band loading.
Cross-training becomes invaluable during this phase. Swimming, cycling at higher cadences with lower resistance, and pool running all maintain cardiovascular fitness without the repetitive impact that aggravates IT band inflammation.
As part of your self-care strategy, consider using a foam roller to target surrounding soft tissues, such as the glutes, TFL, and quadriceps. Foam roll exercises can be beneficial, but avoid aggressive rolling directly over the IT band to prevent worsening the injury.
Running a marathon with IT band syndrome is possible, but requires an honest assessment of where you are in the recovery process and realistic expectations about your performance. Trying to race through active inflammation usually leads to compensatory injuries elsewhere in your body, or forces you to stop partway through, neither of which serves your long-term running goals. If symptoms are resolving and you can complete your long runs without pain, a conservative race strategy with planned walk breaks might allow you to finish while minimizing setback risk.

How Physiotherapy Addresses the IT Band Syndrome
Physiotherapy provides the framework for long-term recovery by identifying and correcting the specific factors contributing to your IT band syndrome. Your physiotherapist starts with a thorough movement assessment, watching you walk, run and perform single-leg tasks. They will assess hip strength, check for tightness in your hip flexors and quadriceps and assess your running form for red flags like crossover gait or an excessive hip drop.
Treatment addresses multiple layers simultaneously rather than focusing solely on the most painful area. The real work is rebuilding the strength and motor control to prevent recurrence. Your physiotherapist will design a progressive exercise program targeting weak hip abductors and external rotators through movements like clamshells, side-lying hip abduction, and single-leg bridges. These aren’t generic stretches. They’re specific corrective exercises that will challenge your current capacity without overwhelming healing tissues.
Manual therapy techniques will release tension in your tensor fasciae latae as they play a key role in stabilizing the IT band and controlling hip movement. Manual therapy also targets hip flexors and vastus lateralis, all muscles that can increase IT band tension when tight. Soft tissue work combined with joint mobilizations will improve hip and knee mechanics, reducing the abnormal forces transmitted through the IT band during movement.

Advanced modalities build on this foundation. INDIBA® uses radiofrequency energy to increase blood flow deep within tissues, accelerating the resolution of inflammation while promoting tissue repair. Unlike superficial heat treatments, INDIBA reaches the exact depth where IT band pathology occurs, making it particularly effective for runners who haven’t responded to conventional approaches. These sessions are painless and can be scheduled around training, if symptoms feel manageable.
Shockwave Therapy delivers acoustic waves that stimulate healing in chronic cases. Mechanical stimulation will break up adhesions, improve local circulation, and trigger the body’s natural repair mechanisms. Many runners notice significant improvement after just a few Shockwave Therapy sessions, especially when combined with a targeted exercise program that addresses their specific weaknesses.
Your physiotherapist will also review your training program and suggest modifications that allow you to continue running while protecting the healing process. This might mean adjusting your weekly mileage progression, varying running surfaces, or incorporating strength work on specific days to optimize recovery. They will teach you to recognize early warning signs so you can back off before minor irritation becomes full-blown inflammation.
Form corrections often play a significant role. Small changes like increasing your cadence by 5-10%, reducing your stride length, or focusing on landing your foot closer to your body’s centre of mass can significantly reduce IT band stress. Your physiotherapist can help you make all these adjustments to your stride.

Preventing IT Band Syndrome From Coming Back
Prevention builds on everything you learn during recovery. The hip strengthening exercises that help you recover need to become part of your routine, not something you abandon once the pain goes away. Most runners benefit from doing targeted hip work 2-3 times a week, adjusting exercises as strength improves to maintain adequate challenge.
Gradual progression is non-negotiable. Even after symptoms resolve completely, gradually increasing mileage and varying your training stress help protect against recurrence. Follow the 10% rule and add mileage on easy runs before pushing pace or distance on strenuous efforts. Build in regular cutback weeks when volume drops by 20-30% to give your body time to adapt to previous training loads fully.
Pay attention to running surfaces and intentionally vary them. Alternate between roads, tracks and trails when possible. If you train on cambered roads, switch which side you run on regularly. During long runs on roads with significant camber, turn around at the halfway point so each leg experiences both the higher and lower side equally.
Replace your running shoes before they’re completely worn out. Degraded cushioning and support alter your mechanics in subtle ways that can restart the cycle of IT band stress. Most runners need new shoes every 400-500 miles, though this varies by body weight, running surface, and individual biomechanics. Your physiotherapist can help guide you if you are unsure of when to change shoes.
Stay in touch with your physiotherapist even after treatment ends. Periodic check-ins allow early identification of emerging weaknesses or form breakdowns before they become problems. Think of these sessions as maintenance rather than injury treatment.

Getting Back to Pain-Free Running
IT band syndrome doesn’t have to stop your training or force you to stop running. This condition responds well to targeted physiotherapy that addresses symptoms and underlying causes.
Whether you’re training for your next race or want to run comfortably around East Coast Park, the proper treatment gets you back on track safely and surely. Don’t try to manage the problem on your own. Get in touch with HelloPhysio to book an appointment and get back to running with ease.